OVERVIEW
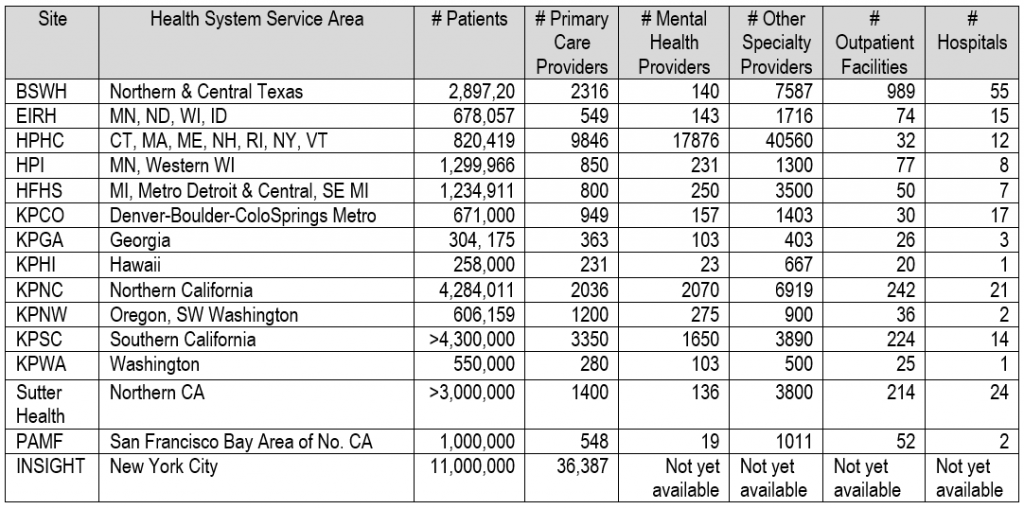
The proposed practice-based research network includes research centers embedded in 21 large integrated health systems serving a combined member/patient population of over 25 million in 16 states. Each health system provides mental health and general medical care to a defined patient population, including substantial numbers from all racial and ethnic groups and substantial numbers insured by Medicaid and other low-income insurance. Below we describe the resources that are available across the network. First, we describe shared resources across all sites, then provide a summary table listing all participating sites with some key health system characteristics, followed by more detailed site-specific characteristics for the care delivery systems, health plans, and research centers.
SHARED RESOURCES
Data Infrastructure
As stated in this proposal, health system clinical and administrative records are necessary but not sufficient for creating a continuously learning healthcare system. Electronic health records (EHRs) and insurance claims data are typically designed as transactional systems to support clinical care and business operations. Unlocking EHR or claims data to support practice-based research requires timely extraction of EHR data, translation to a research-ready common data model, and development of specifications or computable phenotypes to translate individual data elements (e.g. diagnosis codes, NDC/RxNorm drug codes) into clinically meaningful measures and outcomes.
The Health Care Systems Research Network (HCSRN) Virtual Data Warehouse is a highly successful example, facilitating multi-site research while protecting patient privacy and proprietary health practice information, and promoting standardization. Each HCSRN member organization maintains control of its own data via a “distributed” or “federated” model, not a central database. Administrative, clinical, and claims data are translated to a common set of data standards at each site. This model has now been adopted by PCORI’s Clinical Data Research Network and the FDA Sentinel Initiative. Each of the 13 research centers that are currently part of the Mental Health Research Network (MHRN) maintains a research data warehouse (following the HCSRN Virtual Data Warehouse model), including comprehensive, longitudinal data regarding mental health and general medical care.
Virtual Data Warehouse
The HCSRN Virtual Data Warehouse (VDW) currently encompasses twelve data domains. Programmers at each site have transformed EHR, insurance claims, enrollment, demographic, and vital statistics data elements from local data systems to a VDW standardized set of variable definitions, names, and codes. The common structure allows for programming code developed at one site to be used at other sites to extract and analyze data for research. A VDW Operational Committee (VOC) provides direction to each site on the implementation of the VDW. The VOC is also responsible for maintaining current documentation of data availability across sites, including site variations and site-specific issues, quality control evaluation of domain-specific data at each site, and documentation of policies and procedures for initiation and conduct of multi-site research within the HCSRN.
The VDW’s federated model offers an effective means of protecting the identity of patients, providers, and health plans while allowing researchers and analysts to access data from much larger populations than they would otherwise be able to access within their own institution. The VDW serves as the source of standardized data from a variety of data systems in each site (Figure 1).

The VDW includes:
- A series of computerized data sets stored behind separate security firewalls at participating HCSRN sites that include variables with identical names, formats, and specifications and identical variable definitions, labels, coding, and definitions
- A set of informatics tools—hardware and software—that facilitates storage, retrieval, processing, and managing VDW datasets
- A set of access policies and procedures governing use of VDW resources and
- Documentation of all elements of the VDW.
Data standardization involves the following steps:
- Specifying common variable names, labels, coding, and definitions
- Writing parallel programs at each site to extract and convert variables stored in legacy information systems to the common standards
- Testing standardized data for consistency and accuracy
- Standardizing methods by writing macros that are used across projects
- Teaching researchers and their analysts how to use the VDW to guide construction of analysis files for approved research projects.
Syntactic interoperability across sites means a project programmer can use multiple versions of the same data files stored in separate systems to extract and combine information on a selected set of variables and be assured that they have extracted all the available information on these variables from the files and only information on these variables; moreover, these data attributes are homogeneous across settings. Syntactic interoperability is achieved by using the same database and analysis software to store, retrieve, transform, and analyze data from multiple sites and time periods.
Semantic interoperability means that observations from different sites and times represent valid, reliable, and consistent measures of the same underlying well-defined concept across all the sources and over time. This allows investigators to pool the observations on given variables across sites or time. The fundamental rationale for the VDW is to perform all the preparatory work for pooling existing data across multiple sites without creating a single concatenated file stored at one site.
Data Domains within the HCSRN VDW
The data domains within the Virtual Data Warehouse that are available to us in the proposed Program/Project are:
- Demographics contains date of birth, gender, race and ethnicity, and patient language.
- Enrollment is based on health plan membership enrollment or geographic coverage of patients with indicators of insurance types, benefits, and effective dates of coverage.
- Encounters characterizes outpatient visits and inpatient stays, including the associated diagnosis and procedure codes, type of encounter, provider seen, facility, and discharge disposition.
- Procedures consists of all performed procedures including evaluation and management, surgery, laboratory, radiology, and immunization. Currently only performed procedures are captured and include various procedure coding systems (CPT-4, HCPCS, ICD-9-CM, insurance claims Revenue Codes).
- Diagnoses includes dates, diagnosis codes and codes types, primary diagnosis, principal diagnosis flag, and diagnosing provider.
- Providers includes information on the providers such as specialty, age, gender, race, and year graduated.
- Cancer/Tumor Registry based on the Surveillance, Epidemiology and End Results (SEER) program standards as many HCSRN sites are SEER sites. The domain consists of detailed stage and grade, date of diagnosis, dates of treatment initiation, and is one of the most complex domains of the VDW.
- Pharmacy consists of pharmacy dispensing and claims and includes date of dispensing, National Drug Code or GPI code (to standardize across sites), therapeutic class, days-supply, and amount dispensed. These data are widely used to assess pharmacy-based disease and co-morbidity classification systems.
- Vital Signs collected at most in-person encounters and include height, weight, and blood pressure readings. Tobacco use and type are also included.
- Laboratory Results includes clinical laboratory test results for chemistry, hematology and coagulation. Over 100 different lab tests types have been defined for the VDW, but data for every test type is not available at every site. Individual sites have data for the most common test types as well as those high priority tests required for the studies in which they participate.
- Census provides socioeconomic indicators for patient populations based on geocoded patient addresses and public census data, such as rural/urban residence, education level, income, and poverty.
- Mortality includes patient dates of death and causes of death. Mortality data is derived from multiple sources including EHR and utilization data, state death certificate data, and federal death data such as Social Security Administration data and the National Death Index.
Patient-Reported Outcomes – As described in the Overall and Methods Core Application, MHRN researchers have augmented standard HCSRN data tables with tables representing commonly used patient-reported outcome (PRO) measures, including PHQ-2 and PHQ-9 depression scales, GAD-2 and GAD-7 anxiety scales, and AUDIT-C questionnaires regarding alcohol use. These data are stored in the same federated model, with original data tables stored behind firewalls of participating health systems. These tables include responses to individual questionnaire items linked to specific healthcare encounters (e.g. outpatient visits, telephone calls, online portal messages). Across all sites, the number of PHQ-9 observations now exceeds 16 million.
Utilization-Based Denominators – The traditional HCSRN VDW Enrollment table is typically used to define denominator populations based on continuous health insurance enrollment – assuming that all health service use will be captured either by electronic health records (for services provided by the medical group or delivery system) or insurance claims (for services provided by external providers or facilities). This method, however, excludes patients not insured by an affiliated health plan (a large population in some MHRN health systems) and excludes people who are uninsured. Consequently, MHRN has developed and validated utilization-based denominator definitions based on continuity of outpatient service use. We now propose to use these alternative denominator definitions in the INSIGHT network.
Regulatory Compliance and Ethical Oversight
MHRN and the broader Healthcare Systems Research Network have developed a range of resources to ensure regulatory compliance and adequate ethical oversight while minimizing unnecessary delay and expense. Those tools and procedures include:
- IRB Ceding/Reliance Agreements – All members of MHRN/HCSRN agree to follow common streamlined procedures for ceding IRB review or reliance on a single IRB. Single IRB review is routine for studies limited to use of records data and clinical trials using a common protocol at all sites.
- Common online IRB platform – All Kaiser Permanente sites are transitioning to a common online IRB platform (IRBNet), facilitating sharing of documents and researcher credentials and tracking of approvals and expirations.
- Shared review forms and templates – All Kaiser Permanente sites have adopted common forms and templates for IRB application and review.
- Collaborative IRB Workgroup – The HCSRN Asset Stewardship Committee (chaired by Dr. Simon) includes an IRB Workgroup focused on development and improvement of shared procedures and efficient adoption of policy changes (e.g. Common Rule changes, single IRB expectations).
Streamlined Contracting and Fiscal Management Procedures
MHRN has successfully met its contracting and fiscal responsibilities for the past eight years since this network was established in 2010. MHRN and the broader Healthcare Systems Research Network have developed a range of resources to monitor spending, increase transparency, reduce delay, and ensure prudent use of taxpayer resources. Those tools and procedures include:
- Standard subcontract templates – All MHRN/HCSRN sites have adopted standard templates to avoid delays due to case-by-case negotiation of subcontract terms.
- Invoice tracking –Tools have been developed for transparent tracking of invoicing status across MHRN sites to facilitate timely closeout of annual project budgets.
- Monitoring of spend rates – Timeliness of invoicing allows timely tracking of project expenditures, avoiding unexpected fluctuations in spending, avoiding budget shortfalls, and anticipating unspent balances.
PARTICIPATING HEALTH SYSTEMS AND RESEARCH CENTERS
The table below summarizes characteristics of participating health systems. Detailed descriptions of participating health systems, health plans, and research centers follow.
Select Areas of Investigator Expertise
Click on the Institution name to view a detailed description of participating health systems, health plans, and research centers listed below.
| Institution | Investigator | Area(s) of Expertise |
|---|---|---|
| Baylor Scott & White | Katherine Sanchez | Minority health and health disparities Depression treatment |
| Essentia Health | Stephen Waring | Precision medicine / pharmacogenomics Rural health Geriatrics, dementia, multiple comorbidities in elderly |
| Essentia Health | Melissa Harry | Psychometrics Rural health Adolescent mental health Qualitative research Implementation research |
| Harvard Pilgrim | Christine Lu | Pharmacoepidemiology and drug safety Policy analysis and interrupted time series Causal inference in complex observational designs |
| HealthPartners | Rebecca Rossom | Geriatrics Co-occurring mental health and chronic medical illness EHR decision support Neuropsychiatry |
| HealthPartners | Stephanie Hooker | Health behavior change Behavioral health treatment in primary care Motivation, meaning in life, well-being |
| Henry Ford | Brian Ahmedani | Suicide prevention Precision medicine Minority health and health disparities |
| INSIGHT | Jyotishman Pathak | Medical informatics Natural language processing |
| KP Colorado | Arne Beck | Perinatal mental health Implementation research Collaborative care and care management interventions |
| KP Georgia/GSU | Ashli Owen-Smith | Autism Minority health and health disparities Co-occurring mental health and chronic medical illness |
| KP Hawaii | Beth Waitzfelder | Minority health and health disparities Depression, diabetes, cardiovascular disease |
| KP Hawaii | Yihe Daida | Maternal and child health Minority health and health disparities |
| KP Northern California | Stacey Sterling | Co-occurring substance use and mental health disorders Adolescent mental health |
| KP Northwest | Frances Lynch | Health economics Autism Child and adolescent mental health |
| KP Southern California | Karen Coleman | Patient and health system stakeholder engagement Minority health and health disparities Implementation research |
| KP Southern California | Jean Lawrence | Perinatal mental health Adolescent mental health Health behavior change |
| KP Washington | Gregory Simon | Suicide prevention Design and implementation of pragmatic clinical trials Collaborative care and care management interventions |
| KP Washington | Susan Shortreed | Machine learning applications in mental health Causal inference in complex observational designs Design and analysis of pragmatic clinical trials |
| KP Washington | Robert Penfold | Child and adolescent mental health Practice variation and diffusion of innovation Policy analysis and interrupted time series |
| Sutter Health | Ellis Dillon | Implementation research Physician/clinician burnout/well-being research Qualitative/mixed methods research |
Baylor Scott and White Healthcare
Baylor Scott & White Healthcare is a non-profit collaborative health care system in Temple, Texas, encompassing one of the nation’s largest multi-specialty group practices, providing personalized, comprehensive, high-quality care enhanced by medical education and research.
Care Delivery System
- Number of active or affiliated patients: 2,897,202 (‘active patients’ limited to visits in the past 36 months)
- Geographic area served: North Texas: 13 counties, Central Texas: 32 counties
- Number of outpatient facilities: 989 (includes ambulatory care centers, specialty clinics, hospital-based practices, outpatient ancillary, and primary care clinics)
- Number of inpatient facilities: 55 (includes owned, joint venture, affiliated hospitals, and emergency hospitals)
- Number of primary care providers: 2,316 (general practice/family practice/internal medicine physicians – on staff, employed, HTPN, or BSWQA)
- Number of specialty mental health providers: 140
- Number of other specialty providers: 7,587
- EHR system(s) used: Epic
- Date EHR system(s) implemented: Began in 2016, still being rolled out
Health Plan
- Number of enrolled members: Approximately 400,000
- Geographic area served: West, Central, and North Texas
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): It ranges from 0 to approximately 80 percent, depending on geography and line of business.
Research Center
Center for Applied Health Research (CAHR)
- Date founded: August 2010
- Number of current investigators: 4
- Number of current total staff FTE: 16.3
- Approximate annual budget: FY19 $1.9M
- Responsible IRB(s): BSWH IRB
- Active mental health investigators:
- Alan Stevens
- Katherine Sanchez
- Suzy Gulliver
- Eric Meyer
- Keith Young
- Judy Embry
Essentia Health
Essentia Health is an integrated health system headquartered in Duluth, Minnesota; providing comprehensive care to rural communities across the upper Midwest.
Care Delivery System
- Number of active patients (does not include affiliated patients): 554,171
- Geographic area served: Minnesota, North Dakota, Wisconsin
- Number of outpatient facilities: 73 clinics
- Number of inpatient facilities: 13 hospitals
- Number of primary care providers: 443
- Number of specialty mental health providers: 133
- Number of other specialty providers: 1,641
- EHR system(s) used: Epic
- Date EHR system(s) implemented: 2002, but not system-wide in all clinics until 2006 and hospitals until 2014
Health Plan
- Number of enrolled members: n/a
- Geographic area served: n/a
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): n/a
Research Center
Essentia Institute of Rural Health
- Date founded: January 1, 2010
- Number of current investigators: 5
- Number of current total staff FTE: 65
- Approximate annual budget: $14 million
- Responsible IRB(s): Essentia Health IRB
- Active mental health investigators:
- Dr. Stephen C. Waring
- Dr. Irina V. Haller
- Dr. Melissa L. Harry
- Dr. Mark Ham
- Dr. Pat Conway
- Mary McClernon, LICSW
- Dr. Steven Sutherland
- Investigator roles in health system:
- Dr. Stephen Waring – Research Manager
- Dr. Steven Sutherland – Physician Leader
- Mary McClernon, LICSW – Behavioral Health Operations Manager III
Harvard Pilgrim
Harvard Pilgrim Health Care (HPHC) is a large non-profit health plan with diverse enrollees across New England. The Department of Population Medicine (DPM) is a research and academic partnership between Harvard Medical School and HPHC. The DPM resides within the Harvard Pilgrim Health Care Institute (HPHCI) and is an appointing department of Harvard Medical School.
Care Delivery System
- Atrius Health
- Number of active or affiliated patients: 820,419 (406,041 with assigned primary care physician)
- Geographic area served: CT, MA, ME, NH, RI, NY, VT
- Number of outpatient facilities: 32
- Number of inpatient facilities: 12
- Number of primary care providers: 9846 Total (2639 Family Practice, 4116 Internal Medicine, 1943 Pediatrics, 27 Nurse Practitioner, 64 Pediatric Nurse Practitioner, 170 Adult Nurse Practitioner
- Number of specialty mental health providers: 17876
- Number of other specialty providers: 40560
- EHR system(s) used: Epic
- Date EHR system(s) implemented: 2010
Health Plan
- Number of enrolled members: 820,419 as of 3/31/18
- Geographic area served: MA, NH, ME
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): HPHC membership / Atrius health membership overlap estimate: Atrius member of actual members, 72,345
Research Center
Department of Population Medicine, Harvard Pilgrim Health Care Institute
- Date founded: 1992
- Number of current investigators: Faulty: 29, Fellows: 12, Research Scientists: 7 for a total of 48.
- Number of current total staff FTE: 210
- Approximate annual budget: $58 million in external funding, $15 million in organizational funding
- Responsible IRB(s): Harvard Pilgrim Health Care Institutional Review Board, Boston, MA
- Active mental health investigators:
- Christine Lu, PhD
- Stephen Soumerai, PhD
- Frank Wharam, MB, MPH
HealthPartners
HealthPartners is the largest consumer governed non-profit health care organization in the country, providing care, coverage, research, and education to improve the health of its members, patients, and the community.
Care Delivery System
- Number of active or affiliated patients: 1.3 million
- Geographic area served: Minnesota and western Wisconsin
- Number of outpatient facilities: 77 outpatient clinics; 22 urgent care centers; 24 dental clinics
- Number of inpatient facilities: 8 general hospitals; one mental health inpatient facility
- Number of primary care providers: 850
- Number of specialty mental health providers: 231
- Number of other specialty providers: approximately 1,300
- EHR system(s) used: Epic
- Date EHR system(s) implemented: 2005
Health Plan
- Number of enrolled members: 1.8 million medical and dental health plan members
- Geographic area served: Minnesota, Wisconsin, Iowa, Illinois, North Dakota and South Dakota
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): 600,000
Research Center
HealthPartners Institute
- Date founded: 1990
- Number of current investigators: 48
- Number of current total staff FTE: 175
- Approximate annual budget: $40 million
- Responsible IRB(s): HealthPartners Institute IRB
- Active mental health investigators:
- Rebecca Rossom, MD, MS
- Leif Solberg, MD
- Kristin Palmsten, ScD
- Stephanie Hooker, PHD, MPH
- Investigator roles in health system:
- Dr. Rossom: Geriatric Psychiatrist at HealthPartners Medical Group
- Dr. Solberg: Senior Advisor for HealthPartners Medical Group
Henry Ford Medical Group / Henry Ford Physician Network
Henry Ford Health System is a leading health care and medical services provider in the Central and Southeast Michigan region, including Detroit and its metropolitan area, comprised of hospitals, medical centers and one of the nation’s largest group practices, the Henry Ford Medical Group.
Care Delivery System
- Number of active or affiliated patients: 1.25 million
- Geographic area served: Michigan, Metropolitan Detroit and other cities and regions across central and southeast Michigan
- Number of outpatient facilities: 50
- Number of inpatient facilities: 7
- Number of primary care providers: 800
- Number of specialty mental health providers: 110 PhD / MD providers, 250 total providers.
- Number of other specialty providers: 3500
- EHR system(s) used: Epic
- Date EHR system(s) implemented: 2012 (alternate EHR system in use from 1989-2012)
Health Plan
- Number of enrolled members: 750,000
- Geographic area served: Michigan, Metropolitan Detroit and other cities and regions across central and southeast Michigan
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): 125,000
Research Center
Henry Ford Research, Center for Health Policy and Health Services Research
- Date founded: 1915
- Number of current investigators: >200 investigators, including 85 full time investigators and nearly 150 clinician investigators
- Number of current total staff FTE: >500
- Approximate annual budget: $100 million
- Responsible IRB(s): Henry Ford Hospital IRB
- Active mental health investigators:
- Brian Ahmedani
- Lisa Matero
- Jordan Braciszewski
- Michelle Jesse
- Christopher Drake
- Amy Loree
- Investigator roles in health system:
- Dr. Ahmedani is Director of the Center for Health Policy and Health Services Research (CHPHSR) and Director of Research in Behavioral Health Services (BHS)
- Dr. Matero is a scientist in CHPHSR and Director of the Clinical Psychology Fellowship and Internship programs in BHS.
- Dr. Braciszewski is a scientist with appointments in CHPHSR and BHS.
- Dr. Loree is a scientist in CHPHSR.
- Dr. Jesse’s primary appointment is in the Transplant Institute.
- Dr. Drake’s primary appointment is in Sleep Medicine.
INSIGHT Clinical Data Research Network
Care Delivery Systems
- Weill Cornell Medicine
- Columbia University College of Physicians and Surgeons
- Icahn School of Medicine at Mount Sinai Medical Center
- Albert Einstein College of Medicine of Yeshiva University/Montefiore Medical Center
- NYU Langone School of Medicine
- Hospital for Special Surgery
- NewYork Presbyterian
- Number of active or affiliated patients: Approximately 22 million active, approximately 11 million closely affiliated
- Geographic area served: New York City
- Number of primary care providers: 36,487
- EHR system(s) used: Primarily Epic
- Date EHR system(s) implemented: varies by system
Health Plan
INSIGHT CRN has a contractual relationship with HealthCore. HealthCore is an independently operated subsidiary of Anthem Inc. Each of the affiliated medical groups have individual relationships with other health plans.
Research Center
INSIGHT Clinical Research Network
- Date founded: 2013
- Number of current investigators: INSIGHT has supported over 34 studies locally and nationally. It represents 16 academic medical centers and their associated faculty.
- Number of current total staff FTE: 19.5
- Approximate annual budget: $1m (direct costs)
- Responsible IRB(s): Biomedical Research Alliance of New York (BRANY) IRB
Kaiser Permanente Colorado
Kaiser Permanente Colorado is an integrated health care system serving members in the Denver-Boulder-Colorado Springs metropolitan area.
Care Delivery System
Colorado Permanente Medical Group
- Number of active or affiliated patients: 671,000
- Geographic area served: Denver/Boulder metropolitan area, Pueblo, Colorado Springs, Greeley, Loveland, and Fort Collins
- Number of outpatient facilities: 30
- Number of inpatient facilities: Contracted hospitals: Denver/Boulder = 6, Northern Colorado = 4, Southern Colorado = 7
- Number of primary care providers: 949
- Number of specialty mental health providers: 157
- Number of other specialty providers: 1403
- EHR system(s) used: Epic Systems (Madison, WI)
- Date EHR system(s) implemented: 2004
Health Plan
- Number of enrolled members: 671,000
- Geographic area served: Denver/Boulder metropolitan area, Pueblo, Colorado Springs, Greeley, Loveland, and Fort Collins
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): 671,000
Research Center
Kaiser Permanente Colorado Institute for Health Research
- Date founded: 1991
- Number of current investigators: 14 full-time and 10 affiliate MD, PhD, and PharmD investigators
- Number of current total staff FTE: 115
- Approximate annual budget: $17 million
- Responsible IRB(s): KPCO Institutional Review Board
- Active mental health investigators:
- Arne Beck, PhD,
- Jennifer Boggs, PhD
- Sam Hubley, PhD, National Mental Health Innovation Center, Anschutz (affiliate investigator)
- Sona Dimidjian, PhD, Dept of Psychology and Neuroscience, CU Boulder (affiliate investigator)
- Zindel Segal, PhD, Dept of Psychology, University of Toronto (external investigator)
- Jeanette Waxmonsky, PhD, Dept of Family Medicine, UCDHSC (affiliate investigator)
- Bethany Teachman, PhD, Dept of Psychology, University of Virginia (external investigator)
- Danielle Loeb, MD, MPH, Dept of General Internal Medicine, UCDHSC (affiliate investigator)
Kaiser Permanente Georgia
Kaiser Permanente Georgia (KPGA) operates outpatient medical facilities throughout metropolitan Atlanta. The Center for Research and Evaluation at KPGA has as its mission to engage in clinical, epidemiologic, and health services research to advance basic science and contribute to KPGA quality improvement initiatives.
The Southeastern Permanente Group (TSPMG)
Care Delivery System
- Number of active or affiliated patients: 304,175
- Geographic area served: Georgia
- Number of outpatient facilities: 26
- Number of inpatient facilities: 3
- Number of primary care providers: 363
- Number of specialty mental health providers: 103
- Number of other specialty providers: 403
- EHR system(s) used: Epic/KP Health Connect
- Date EHR system(s) implemented: 2003
Health Plan
- Number of enrolled members: 304,175
- Geographic area served: Georgia
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): 304,175 (~100%)
Research Center
Kaiser Permanente Georgia – Center for Research and Evaluation
- Date founded: 1998
- Number of current investigators: 4 Full-Time; 2 Affiliate; 5 Adjunct
- Number of current total staff FTE: 21
- Approximate annual budget: $2 million
- Responsible IRB(s): Kaiser Permanente Georgia
- Active mental health investigators: Ashli Owen-Smith, PhD
Kaiser Permanente Hawaii
The Center for Health Research, Hawaii (CHRH) is located on Honolulu, HI. The strategic focus is to “advance knowledge to improve the health of diverse populations”.
Hawaii Permanente Medical Group (HPMG)
Care Delivery System
- Number of active or affiliated patients: 251,000
- Geographic area served: Hawaii
- Number of outpatient facilities: 20 primary care clinics
- Number of inpatient facilities: 1 – Moanalua on Oahu and 24 affiliated hospitals on all islands for inpatient services
- Number of primary care providers: 231
- Number of specialty mental health providers: 23
- Number of other specialty providers: 667
- EHR system(s) used: EPIC (KP HealthConnect)
- Date EHR system(s) implemented: 1996
Health Plan
- Number of enrolled members: 251,000
- Geographic area served: Hawaii
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): 251,000
Research Center
Center for Health Research, Hawaii (CHR-H)
- Date founded: 1999
- Number of current investigators: 5
- Number of current total staff FTE: 30
- Approximate annual budget: $6 million
- Responsible IRB(s): Kaiser Permanente Hawaii Institutional Review Board
- Active mental health investigators:
- Beth Waitzfelder, PhD
- Yihe Daida, PhD
- Vanessa Simiola, PsyD
Kaiser Permanente Northern California
Kaiser Permanente Northern California Division of Research(DOR) was established in 1961 as a department within The Permanente Medical Group of Kaiser Permanente in Northern California serving as the principal consulting resource for health services and clinical studies for Kaiser Permanente Northern California, one of the largest health care delivery organizations in the U.S.
The Permanente Medical Group
Care Delivery System
- Number of active or affiliated patients: 4,284,011
- Geographic area served: Northern California
- Number of outpatient facilities: 242
- Number of inpatient facilities: 21
- Number of primary care providers: 2,036
- Number of specialty mental health providers: 2,070
- Number of other specialty providers: 6,919
- EHR system(s) used: EPIC (KP HealthConnect)
- Date EHR system(s) implemented: 2004
Health Plan
- Number of enrolled members: 4,284,011
- Geographic area served: Northern California
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): 4,284,011
Research Center
The Division of Research
- Date founded: 1961
- Number of current investigators: 58
- Number of current total staff FTE: 600
- Approximate annual budget: $90 million
- Responsible IRB(s): Kaiser Permanente Northern California Institutional Review Board
- Active mental health investigators:
- Stacy Sterling, DrPH, MSW
- Derek Satre, PhD
- Lisa Croen, PhD
Kaiser Permanente Northwest
Kaiser Permanente Northwest (KPNW) is one of eight regions of the Kaiser Permanente Medical Care Program; providing medical and dental insurance coverage to members in northwest Oregon and southwest Washington. The Center for Health Research (TCHR) is a non-profit research institute closely affiliated with Kaiser Permanente Northwest (KPNW).
Northwest Permanente Medical Group
Care Delivery System
- Number of active or affiliated patients: 606,159
- Geographic area served: Oregon, Southwest Washington State
- Number of outpatient facilities: 36
- Number of inpatient facilities: 2
- Number of primary care providers: 1,200 physicians total
- Number of specialty mental health providers: 275 (includes all types, not just physicians)
- Number of other specialty providers: 900
- EHR system(s) used: Epic
- Date EHR system(s) implemented: 1996
Health Plan
- Number of enrolled members: About 600,000
- Geographic area served: Oregon, Southwest Washington State
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): approximately 85%
Research Center
Kaiser Permanente Center for Health Research
- Date founded: 1964
- Number of current investigators: 41
- Number of current total staff FTE: 242.11
- Approximate annual budget: 45 million
- Responsible IRB(s): Kaiser Permanente Northwest Institutional Review Board
- Active mental health investigators:
- Frances Lynch, PhD, MSPH
- Gregory Clarke, PhD
- Bobbi Jo Yarborough, PsyD
- John Dickerson, PhD, MS
- Nangel Lindberg, PhD
Kaiser Permanente Southern California
Kaiser Permanente Southern California Department of Research and Evaluation manages all research within Kaiser Permanente Southern California, located in Pasadena, California, which is located centrally within the Southern California region.
Care Delivery System
- Number of active or affiliated patients: 4.3 million +
- Geographic area served: Southern California which includes the following counties – Kern, Los Angeles, Orange, Riverside, San Bernardino, San Diego and Ventura counties
- Number of outpatient facilities: 224
- Number of inpatient facilities: 14
- Number of primary care providers: Approx. 3350
- Number of specialty mental health providers: Approx. 1,650
- Number of other specialty providers: Approx. 3890
- EHR system(s) used: Epic
- Date EHR system(s) implemented: 2004
Health Plan
- Number of enrolled members: Approximately 4.3 million
- Geographic area served: Southern California which includes the following counties – Kern, Los Angeles, Orange, Riverside, San Bernardino, San Diego, and Ventura counties
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): Approximately 4.3 million (all)
Research Center
Kaiser Permanente Department of Research & Evaluation
- Date founded: 1958
- Number of current investigators: 32 Research Scientist/Investigators, 3 Research Fellows, 8 Clinical investigators, 21 Affiliated Investigators
- Number of current total staff FTE: 300+
- Approximate annual budget: 57 million
- Responsible IRB(s): Kaiser Permanente Southern California (KPSC) Institutional Review Board (IRB)
- Active mental health investigators:
- Karen J. Coleman
- Jean Lawrence
- Rulin C. Hechter
- Corinna Koebnick
- Darios Getahun
- Reina Haque
- Erin Hahn
- Claudia Nau
- Investigator roles in health system:
- Karen J. Coleman – Evaluation Specialist, Department of Clinical Analysis Southern California Permanente Medical Group, Pasadena, CA
- Erin Hahn – Health Services Research Endowment, Kaiser Permanente Southern California Health Plan, Pasadena, CA
Kaiser Permanente Washington
Kaiser Permanente Washington (KPWA) is a nonprofit health system based in Seattle, Washington, providing coverage and care for people in Washington state. Kaiser Permanente Washington Health Research Institute (KPWHRI) is the research center embedded within KPWA. KPWA is serving as the prime site for this grant application.
Washington Permanente Medical Group
Care Delivery System
- Number of active or affiliated patients: 550,000
- Geographic area served: Washington state
- Number of outpatient facilities: 25
- Number of inpatient facilities: 1
- Number of primary care providers: 280
- Number of specialty mental health providers: 28 psychiatrists and 75 psychotherapists
- Number of other specialty providers: 500
- EHR system(s) used: Epic
- Date EHR system(s) implemented: 2005
Health Plan
- Number of enrolled members: 710,000
- Geographic area served: Washington state
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): 450,000
Research Center
- Kaiser Permanente Washington Health Research Institute
- Date founded: 1984
- Number of current investigators: 60
- Number of current total staff FTE: 300
- Approximate annual budget: 52 million
- Responsible IRB(s): Kaiser Permanente Washington Human Subjects Review Committee
- Active mental health investigators:
- Gregory Simon, MD, MPH
- Robert Penfold, PhD
- Susan Shortreed, PhD
- Yates Coley, PhD
- Kathy Bradley, MD, MPH
- Cara Lewis, PhD
- Investigator roles in health system:
- Gregory Simon practices in Behavioral Health Service
Sutter Health
Sutter Health is a multi-specialty, non-profit organization serving patients in counties in Northern California.
Care Delivery System
- Number of active or affiliated patients: 3,000,000
- Geographic area served: Northern California
- Number of outpatient facilities: 214
- Number of inpatient facilities: 24
- Number of primary care providers: 1,400
- Number of specialty mental health providers: 136
- Number of other specialty providers: 3,800
- EHR system(s) used: Epic
- Date EHR system(s) implemented: 2000 (outpatient) 2012 (inpatient)
Health Plan
- Number of enrolled members: N/A
- Geographic area served: N/A
- Approximate number of health plan members receiving all or most care through affiliated medical group(s): N/A
Research Center
Palo Alto Medical Foundation Research Institute
- Date founded: 1930
- Number of current investigators: 9
- Number of current total staff FTE: 61
- Approximate annual budget: 11.7 million
- Responsible IRB(s): Sutter Health IRB
- Active mental health investigators:
- Ellis Dillon, Ph.D.
- Kristen Azar, RN, MSN/MPH
